A Unique Suicide Risk Screening Tool
The Columbia Protocol, also known as the Columbia-Suicide Severity Rating Scale (C-SSRS), supports suicide risk screening through a series of simple, plain-language questions that anyone can ask. The answers help users identify whether someone is at risk for suicide, determine the severity and immediacy of that risk, and gauge the level of support that the person needs. Users of the tool ask people:
- Whether and when they have thought about suicide (ideation)
- What actions they have taken — and when — to prepare for suicide
- Whether and when they attempted suicide or began a suicide attempt that was either interrupted by another person or stopped of their own volition
Using the Columbia Protocol
Asking Questions
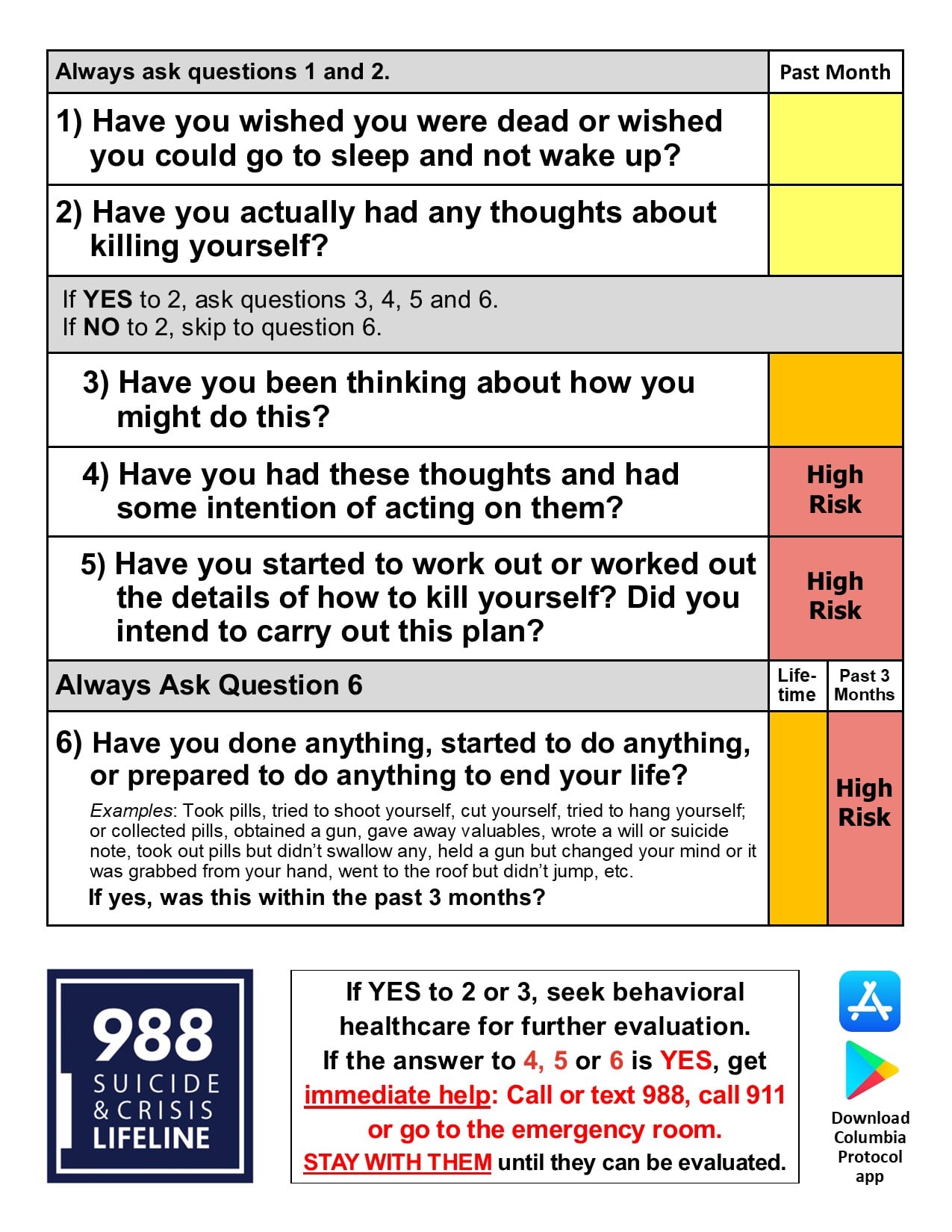
Protocol administrators ask a series of questions about suicidal thoughts and behaviors. The number and choice of questions they ask depend on each person’s answers. The questioner marks “yes” or “no,” as well as how recently the thought or behavior occurred and a scoring of its severity. The shortest screeners are condensed to a minimum of two and a maximum of six questions, depending on the answers, to most quickly and simply identify whether a person is at risk and needs assistance. For a more thorough risk screening, Columbia Protocol askers should use the standard scale.
The Columbia Protocol questions use plain and direct language, which is most effective in eliciting honest and clear responses. For example, the questioner may ask:
- “Have you wished you were dead or wished you could go to sleep and not wake up?”
- “Have you been thinking about how you might kill yourself?”
- “Have you taken any steps toward making a suicide attempt or preparing to kill yourself (such as collecting pills, getting a gun, giving valuables away, or writing a suicide note)?”
Determining Next Steps
To use the Columbia Protocol most effectively and efficiently, an organization can establish criteria or thresholds that determine what to do next for each person screened. Decisions about hospitalization, counseling, referrals, and other actions are informed by the “yes” or “no” answers and other factors, such as the recency of suicidal thoughts and behaviors.
The Columbia Lighthouse Project provides many examples of triage documents that Columbia Protocol users in hospitals, primary care practices, behavioral health care facilities, military services, prisons, and other settings employ to make these decisions. The Project also provides assistance to any organization that is thinking through its policy and establishing a care plan.
Endorsed, Recommended, or Adopted by:





Suicide Prevention Benefits
The first step in effective suicide prevention is to identify everyone who needs help. The Columbia Protocol was the first scale to address the full range of suicidal thoughts and behaviors that point to heightened risk. That means it identifies risk not only if someone has previously attempted suicide, but also if he or she has considered suicide, prepared for an attempt (for example, buying a gun, collecting pills, or writing a suicide note), or aborted plans for suicide because of a last-minute change of mind or someone’s intervention.
The Columbia Protocol screens for this wide range of risk factors without becoming unwieldy or overwhelming, because it includes the most essential, evidence-supported questions required for a thorough screening. The Columbia Protocol is:
- Simple. Ask all the questions in a few moments or minutes — with no mental health training required to ask them.
- Efficient. Use of the protocol redirects resources to where they’re needed most. It reduces unnecessary referrals and interventions by more accurately identifying who needs help — and it makes it easier to correctly determine the level of support a person needs, such as patient safety monitoring procedures, counseling, or emergency room care.
- Effective. Real-world experience and data show the protocol has helped prevent suicide.
- Evidence-supported. An unprecedented amount of research has validated the relevance and effectiveness of the questions used in the Columbia Protocol to screen for suicide risk, making it the most evidence-based tool of its kind.
- Universal. The Columbia Protocol is suitable for all ages and special populations in different settings and is available in more than 150 country-specific languages.
- Free. The protocol and the training on how to use it are available free of charge for use in community and healthcare settings, as well as in federally funded or nonprofit research.
Origins of the Columbia Protocol
Columbia University, the University of Pennsylvania, and the University of Pittsburgh — supported by the National Institute of Mental Health (NIMH) — developed the screening tool for a 2007 NIMH study of treatments to decrease suicide risk among adolescents with depression. The Columbia Protocol, based on more than 20 years of scientific study, filled an urgent need for suicide research and prevention: a better way to uniformly and reliably identify people who are at risk. The Columbia Protocol achieved accurate and comparable results by using consistent, well-defined, and science-based terminology. Just as important as its ability to identify who might attempt suicide, it was the first tool to identify the full range of a person’s suicidal ideation and behavior, including intensity, frequency, and changes over time. .
In 2011, the Centers for Disease Control and Prevention adopted the protocol’s definitions for suicidal behavior and recommended the use of the Columbia Protocol for data collection. In 2012, the Food and Drug Administration declared the Columbia Protocol the standard for measuring suicidal ideation and behavior in clinical trials. Today, the Columbia Protocol is used in clinical trials, public settings, and everyday situations, such as in schools, faith communities, hospitals, and the military, to identify who needs help — saving lives in 45 nations on six continents.